NHS Continuing Healthcare: 9 practical tips

9 insights to help you with NHS Continuing Healthcare
One of our readers, Nick, wrote to us about NHS Continuing Healthcare: he shares his 9 practical tips – to help other families going through the nightmare Continuing Healthcare application process.
Nick’s case involved his father. (Nick’s name has been changed for reasons of confidentiality.)
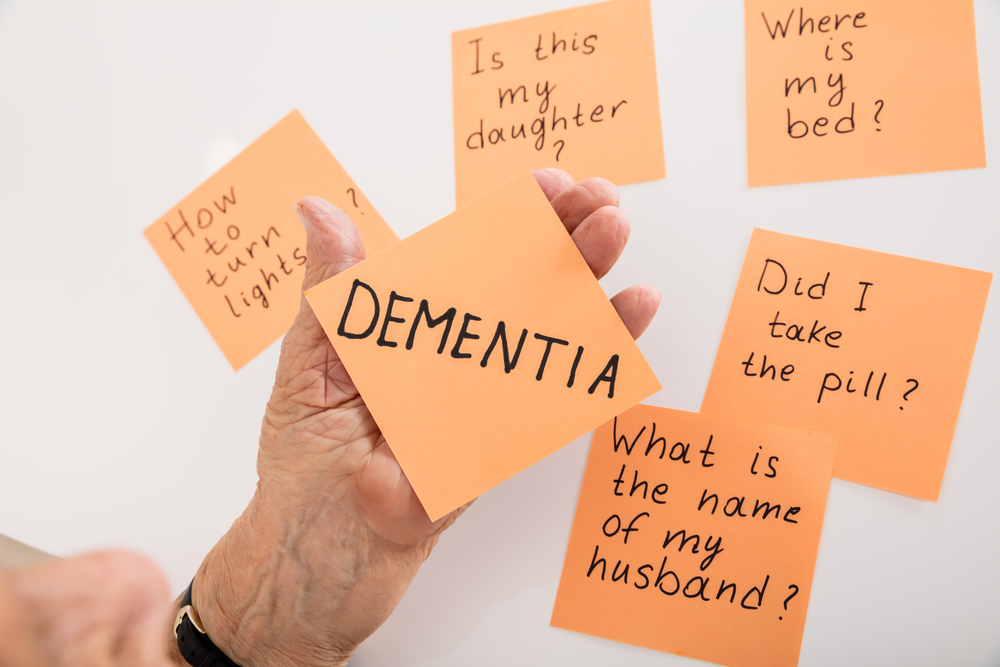
His father’s cognition had been gradually deteriorating over the last year or so, but then took a sharp turn for the worse. His father’s behaviour then became extremely challenging, posing a serious risk to both himself and others.
His father has sadly now died, but Nick has kindly shared his tips and advice here, based on his own personal experience trying to make sense of the Continuing Healthcare application process.
He continues…
NHS Continuing Healthcare: 9 practical tips
1. One of the things I’d like to reinforce is the issue of being dispassionate during the Continuing Healthcare application process – and in care situations in general. It is difficult and yet important. When I say dispassionate, I means towards your parent/relative and their suffering in order to be able to ‘hold the line’ with the authorities. We should have delayed my father’s discharge from the mental hospital into the care home. This happened straight after he had started on antipsychotic drugs, but no time had been given to see how he would react to them. Once we were out of the NHS system we had little or no leverage. I also noticed I felt guilty about ‘bed blocking’ and yet also had the feeling of David trying to hold the line with Goliath.
2. The level of manipulative behaviour and downright lying on the part of NHS staff to try to avoid NHS accountability for my father’s care was shocking, so be prepared for this.
3. I don’t think there is a substitute for reading from cover to cover the National Framework for NHS Continuing Healthcare as well as the Checklist and Decision Support Tool documents. Although it was painful for me to have read all that stuff, I was able to highlight what I considered to be relevant sections. I stapled in tabs on the various pages I’d highlighted and even labelled those tabs with a note about what a particular paragraph was about. I then always carried these documents in a file. Every time I saw Dad I had it with me, with the expectation that if I needed to ‘educate’ somebody about the process I could just pull out the documentation and show them. This had the impact of lessening my anxiety going in to see Dad because I felt better armed should I be approached. It also enabled me to evidence my position rather than being for the most part in a situation where I would say one thing and the NHS staff another – which meant nothing would happen.
4. There is a quick reference guide to the National Framework that I found useful as well. It helped me interpret all the jargon.
5. There’s a really useful diagram on page 23 of the National Framework guidelines. I wish I’d come across that earlier. Perhaps it’s the way I learn things, but the flow chart of the whole NHS Continuing Healthcare assessment process really helped give me clarity and cut through the complexity of all the stages around eligibility. I believe just showing that to an ‘uninformed’ member of NHS staff would in of itself be useful as a way of clarifying or overcoming some of the misinformation around Continuing Healthcare.
6. Another insight that wasn’t clear to me initially, was that fundamentally the information gathered via the Checklist and Decision Support Tool provides evidence around the four characteristics of need: of nature, intensity, complexity and unpredictability. I hadn’t realised this linkage early on and had been trying to figure out how these were connected.
7. Without help, it’s difficult for most people to score the Checklist and not be bamboozled by NHS staff. I have no solution for that.
8. Something of a quick and dirty test that was really useful was this: if your relative doesn’t have money, would social services be willing to care for him? Of course the answer in our case would have been no, and just knowing that was somehow reassuring to potentially help cut through scores on domains etc.
9. Another point that was useful to know was about Dad’s sectioning. By being sectioned under Section 2 the NHS was covering itself against future financial liability for his ongoing care, rather than by sectioning him under Section 3. A Section 2 can only last one month and we were curious to see what would happen after that month. What they did was to remove the section and instead hold him under the Mental Health Act – to avoid any ongoing financial liability. Otherwise they would have had no choice but to resection him under Section 3. Very crafty and it is happening much more.
———-
If you can relate to these points from your own family’s experience, please share your thoughts and insights below.

Sensible advice from Nick. When we started down this route to attempt to secure funding for my Mum, I did not immediately realise how important it was to be familiar with the National Framework but quickly understood I would be on a fast learning curve. Having ‘earned’ the ability to attend the Decision Support Tool (DST) meeting (the first having been held without me there) and prepared questions about relevant points in the National Framework, I discovered that there was no copy of the Framework routinely brought to the meeting by any of the professionals present. It was abundantly clear that they did not expect to answer relevant questions. I asked for a pause and for a copy to be brought into the meeting. This at least was agreed. This was over a year ago now and we are waiting for an Independent Review Panel on appeal. I would urge anyone with responsibility for helping a relative or friend to pursue funding to follow Nick’s suggestions. I would also suggest that if you do prepare questions or raise points, that you ask for these to be recorded by the meeting, take the initiative to provide a written copy of your points for the DST and ask for this also to be incorporated in the record. That way any remarks you make should not be be disputed.
I can relate to Nick’s experience completely. When Dad’s mental health was poor and he developed difficult, challenging and sometimes aggressive behaviour a police officer informed us he would not be sectioned as no-one was anymore as there were no mental health beds.
Referred to the psychiatric hospital – on our insistence after nearly 3 weeks of ‘bedblocking’ in a general hospital after walking in front of a car- this hospital then transferred him without our knowledge to a dementia unit. After a few days of explaining that we wanted support to look after him at home as he was unmanageable due to his mental state – this unit began to talk about ‘a best interests meeting’. Dad was miserable and frightened in the unit so we simply took him home. The meeting was cancelled and the NHS no longer had a problem. They knew how severely ill he was but offered nothing and the discharge process simply involved giving us a carrier bag with his clothes in and lots of bottles of shower gel and hair conditioner with his name on that were not his. There was no assessment of any kind for Continuing Healthcare (CHC) or anything else. They believed he needed 24 hours care but made no effort to find out whether we felt willing and able to provide this without help. Once back home he was simply not an NHS problem anymore and was simply referred to social services who spent 6 months trying to persuade us to have a financial assessment, this was the most important assessment they repeatedly told us. Eighteen months on he continues to get worse and is now seriously ill with an infection and sepsis and we continue to provide all care with the help of a private paid carer. Almost 18 months since he was discharged from hospital he is now facing the CHC assessment. A social worker visited and a psychiatrist but unfortunately their questions have deepened his depression and anxiety as he believes that they are trying to get him locked away.
As Nick writes, the way NHS staff behave is quite shocking and I have found it difficult to explain to friends when they ask how dad is – they simply don’t believe that doctors and nurses are capable of such behaviour. To deny assessment, to deny care, to discharge and avoid any responsibility seem to be their guiding principles. The well-being and health of the patient is simply not their priority.
Yes exactly the same thing happened with my Dad – sectioned under section 2 and then when it ran out held for another month on a Deprivation of Liberty order, yes very crafty – he also has terminal cancer as well as dementia and the place at the secure unit was costing the NHS about £4000 a week – I avoided all questions re property etc and he was Fast Tracked to a nursing home on the advice of the consultant. The nursing home is very good and specialist dementia place so at the 12 week review they decided he no longer qualified for Continuing Healthcare (CHC) and withdrew funding (needs well managed). I have appealled and have since learnt from the home that payment has stopped – I assumed that they had to continue to pay pending appeal – even the home seemed to think this is the case. They are now dragging their heels with the appeal – does anybody else have any experience of who pays when an appeal is in process?
As Nick says when it comes to care for the elderly everything is underhand and you can’t trust “professionals”.
Today I updated the social worker, who is due to attend the Continuing Healthcare (CHC) assessment next month, with dad’s recent deterioration, infection, sepsis, complete loss of mobility, delirium and the community nursing team arranging a hospital bed and hoist as we can’t lift him – and her comment ? The bed “will lessen the number of falls out of bed” . She is, as they all are, simply determined to deny that he has any needs and to trivialise and dismiss any needs we describe. So his health has deteriorated significantly and he could be dying and yet instead of suggesting Fast Track she calculates that he may now suffer from fewer falls because he can’t walk any more.
She answered my email by thanking me for informing her of “how he was currently presenting” – presumably so she can say that he doesn’t always present this way – and described his serious illness as “a very quick infection”. The doctor regarded it as very serious, particularly given my father’s age and frailty, and yet the Social Worker, who has no medical training, is happy to dismiss it and concentrate instead on the fact that he might fall out of bed less often. How do these people sleep at night?
This is appalling to think these stressful situations are happening all over the country. I had to fight long and hard for Continuing Healthcare funding for my mother last year and although I was successful she only benefitted from it for the last 12 weeks of her life. She had Motor Neurone Disease which meant she could not lift a finger to scratch an itch, blow her nose, hold a cup and drink, walk, turn over in bed etc etc. Plus she was having psychological problems being trapped in her body whilst her brain was fully functional. – she was petrified of her impending death. Luckily I had worked in the NHS for 20 years and I downloaded the criteria and the NSF so knew what I was going into. During the scoring I was incensed when the NHS worker said as she was being hoisted she was mobile even though she had fallen 6 weeks before and broken her neck! What are these people doing working in the NHS. Something needs to change regarding this situation. The NHS and Social Services (funded by the local Council) should have their funding Ring-fenced and the Government should be putting more funds into the pot for the elderly. I am now faced with the same situation for my 90 year old father.
Parent is 100% NHS Continuing Healthcare (CHC) funded. Since regulated agencies taken on care, quality of life has eroded. Now being kept in bed – even when asks for toilet (to have bowel movement) we have to lie saying toilet broken and instruct to do in incontinence pad. Yet NHS and agency say they are looking after this guy in his best interest. Deprivation of liberty and against basic human rights. The more I battle, the more hostile NHS is.
Mum got full funding – went for the review and was told that as her pressure sores were now healed she no longer was eligible for full funding. Mum is completely paralysed from the waist down so has to be hoisted she is also on high doses of morphine and scored High on everything but they scored her Low on pressure sores. I am going back for another full assessment in 3 weeks. Can anyone tell me how the social workers can downgrade her when the only reason she does not have the bed sores any more is because of the care she is getting. Also how do I appeal if turned down again?
I completely agree with Nick’s comments. My own mother died in February, following 10 weeks of hell in a local cottage hospital. When admitted, she was suffering from recurring kidney infections (diagnosed with end stage kidney disease 18 months ago), incontinent, virtually no mobility, almost totally deaf. I had looked after her at home with the help of paid carers for as long as I could, but it became impossible for us all. She was given a Checklist assessment for Continuing Healthcare (CHC) which pronounced she had no mobility problems, and no other issues that warranted CHC(!). I challenged this successfully and the forms were submitted for a full assessment. This was just the start of a 10-week battle to get the help she needed. The staff pressured me constantly to take her home. I refused to allow her to be discharged without a full assessment, a date was set, then postponed indefinitely! They then changed tack and advised me to put Mum in a nursing home – I was told this was a special ‘discharge and assess’ procedure, there was nothing to worry about, Mum would be assessed in the nursing home. I was rightly suspicious and refused point blank to let them discharge her until the full assessment had been carried out. While all this was going on, Mum’s health was steadily getting worse, the care she received was minimal, and in the end she died before anything else could be done. Four months on, I remain appalled at the downright lies I was told about the procedure for CHC funding. Had it not been for Care to be Different and everything I learned from this website, I would probably just have accepted all the downright lies I was told, although not the callous indifference I encountered. People who refer to the ‘Caring NHS’ clearly have not encountered NHS ‘care’ for the elderly! I feel guilty that all my efforts to help my mother came to nothing in the end, but I would do the same again if I had to. I found Angela’s e-book How to Get the NHS to Pay for Care invaluable, and recommend it to anyone going through this harrowing process.
The Sectioning aspect is very interesting. My wife was detained under a Section 2 order but spent 9 weeks in a mental health facility while they experimented with different anti-psyshotic medications. Surely she should have been automatically placed on a Section 3 order after the 28th day or allowed home. I am desperate for any legal clarity on this because a Section 3 entitles a person to NHS Continuing Healthcare straight away. I’ve been fighting the CHC for 7 years now without success. They seem to be oblivious, or ignorant, about the High Court decision to set a benchmark standard of care entitlement established in the Coughlan case.Please help us with any relevant comments on this important matter.
Dad was on a section 2 at the hospital. then down graded to a Deprivation of Liberty Safeguard (DoLS). I was told he needed a nurseing home rather than a care home. he had been admitted to the hospital as he had attacked two members of staff knocking one out/ there had been previous incidents at the home and the police had been called. The hospital said the care home was incompetant and that a nursing home would cope with his needs. He went to the nursing home on 5/6/17 and on 8/6/17 without my knowledge only after the event. employed a one to one care currently for 11 hours per day. The care cost has now doubled to 3046 pounds per week. and the house is not sold yet. The nursing home said the hospital lied to them on there assessment and they records arrived a week after my dad. The other day whilst the one to one was in attendance he attacked another member of staff punching her and pulling her hair. I had voiced my concerns to the hospital but i was ignored. Can any one help me – thanks jackie
There seems to be much discussion on this thread about how various patients have not been “sectioned” under the correct part of the Mental Health Act 1983.
My understanding is that it is “unofficial” policy of the Department of Health/NHS England to clinicians that make decisions about whether or not to section patients under section 3 of the Mental Health Act 1983 that clinicians should avoid doing so unless it is absolutely necessary.
The reason for this “unofficial” policy is that the Department of Health/NHS England and the clinicians who make the day to day decisions know full well that if a patient is sectioned under the relevant provision of the Mental Health Act 1983 it means that the National Health Service would be obliged to meet the continuing healthcare funding of that patient indefinitely.
That is why detention under section 2 of the Mental Health Act is far more common than detention under section 3.
It is quite wrong, and clinicians should be doing what is in the best interests of their patients medically. And of course, not all patients will require ongoing “aftercare” of the type envisaged by section 117 of the Mental Health Act 1983. However, no one should be surprised or under any illusions that this “unofficial” policy is being implemented, given that sectioning a patient has the potential to increase NHS Continuing Healthcare costs significantly and given that the NHS finds itself in a funding crisis.
Today the National Audit Office (“NAO”) has now published its report on NHS Continuing Healthcare (“NHSCHC”).
As well as highlighting problems patients and their relatives have accessing the system the NAO report says the bill for NHSCHC was believed to be £3.607 billion in 2015/17 and is estimated to grow to £5.247 billion by 2020/21.
The NAO report also says NHS England wants clinical commissioning groups (“CCGs”) to make £855 million of savings in NHSCHC and NHS-funded nursing care by 2020-21 based on the projected future increase in costs.
The NAO report says NHS England assumes increasing both consistency (presumably consistency in the interpretation of the Department of Health’s (“DoH”) National Framework guidance, the DoH’s Checklist and Decision Support Tool) and the number of patients assessed after being discharged from hospital will result in CCGs providing NHSCHC funding to FEWER patients overall compared with NHS England’s predicted growth in eligibility.
To be fair, the NAO report also says that savings will also be found through better commissioning of care packages and reducing the costs of making assessments of NHSCHC.
However, the mind boggles as to how CCGs intend to come up with ever more cunning ways NOT to follow the legally binding judgement of the Court of Appeal in R. v. North and East Devon Health Authority, ex parte Coughlan to reduce the number of people eligible!
We had Mum’s Decision Support Tool (DST) meeting today and were informed Mum does qualify for full NHS Continuing Healthcare (CHC) funding (much to our surprise!). However, we are concerned about the continuous reviews that will take place, as I have every suspicion that the NHS will look to get out of their obligations asap. Mum has mixed Dementia and is unlikely to get better, however the Representative from the CCG informed us that once she becomes ‘less mobile’ they may well decide that her care needs have reduced and funding could be removed. My question is: Mum isn’t able to self-fund, so if NHS funding is removed later on, who will pick up the cost of the care home? Would this automatically fall to the Local Authority who are already aware that Mum isn’t a self-funder? We aren’t in a position to pay anything towards care home costs either, and are worried what might happen if we are landed with a huge bill none of us can pay. Any advice gratefully received.
Have requested an NHS Continuing Healthcare assessment, I have been told it will be a long time before we get one as there’s a waiting list ……am main carer for friend with young onset alzheimer’s, and have LPA for her. The consultant and mental health nurse said “she’s not eligible as she owns her own house” ………have put them right on that point, thanks to this wonderful site .
The mental health nurse came this week and took notes to fill in a form ……to aid the assessment . Have just received a copy of it via email for me to check through before she sends it off …….. it’s a Specialist Assessment for Complex and Nursing Needs form. Any hints and tips about this form which I need to be aware of, or, wary of before I agree to it being sent off please ?
Thanks.